Just in time for Bowel Cancer Awareness month, I thought I would start off my first blog series on gut health – specifically, the gut microbiome (or gut bacteria).
Did you know that bowel cancer is the second most common type of cancer in Australia? Of all diagnosed cases, 30% of people typically have a family history of the condition. However, apart from genetic factors, recent research has shown that certain microbiota (including in the mouth) may also impact our risk for bowel cancer.
Microbiota are the bacteria living in our digestive tract, from the mouth right down to the rectum. They help to maintain the ‘environment’ in our gut, and humans have an estimated 100 trillion bacteria in the intestine. Different types or amounts of microbiome can cause an imbalanced ‘environment’, and can not only impair digestive function, but may also cause symptoms like constipation, diarrhoea and bloating.
Microbiota help to maintain the ‘environment’ in our gut’, and humans have an estimated 100 trillion bacteria in the intestine.
While we may be born with certain types of microbiome (dependent on genetics and parents’ lifestyle at conception), these gut bacteria regularly change. Diet is something that can greatly influence the types and amounts of bacteria in your gut.
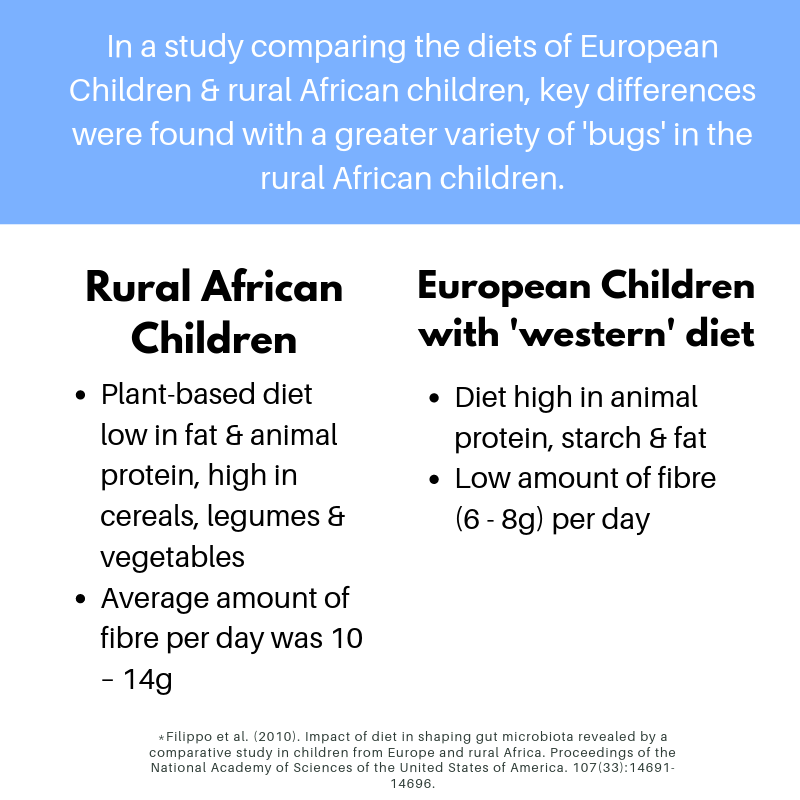
For example, in a study comparing the diets of European children and rural African children, key differences were found with a greater variety of bacteria in the rural African children. These children had a higher biodiversity of gut bacteria, including those related to anti-inflammation and protecting against bowel diseases.
Another review by Yang & Yu compiled the results from several different human and animal studies and found that fibre, protein and fat intake were the main influencers to gut microbiota. The key points were:
- The fermentation of fibre in the large intestine produces short-chain fatty acids (SCFAs), particularly butyrate. This acts as ‘food’ for the cells in the colon and promotes anti-inflammatory actions.
- High intakes of animal protein did not change the variety of microbiota but did cause protein fermentation and bile acid deconjugation, which in turn increased inflammation of the colon.
- Diets high in fat, particularly from processed meats and red meat, increased the release of bile acids, which damaged the lining of the intestines.
- There were conflicting studies on whether processed meat and red meat consumption caused increased risk for developing bowel cancer; however, most of the current evidence suggests that there is an increased risk.
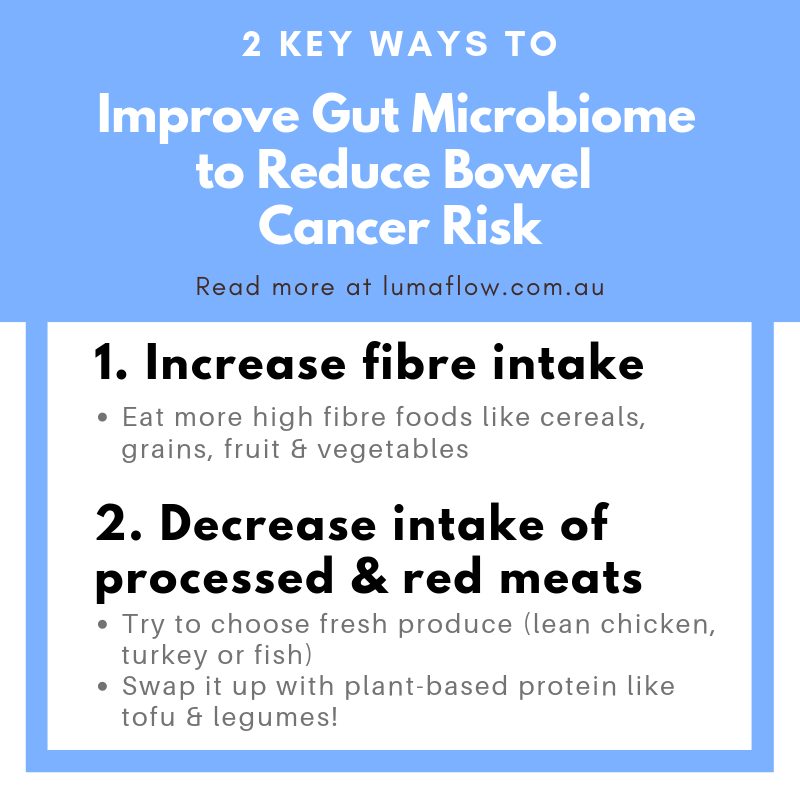
So, it seems like the biodiversity or variety of microbiota is important in helping to reduce the risk of bowel cancer, as is reducing inflammation in the colon. What things can we do to improve the amount and variety of gut bacteria and reduce the risk of inflammation?
Two key methods stood out based on the above research:
-
Increase fibre intake
-
Decrease intake of processed and red meats
This post was a nerdy summary of the current scientific evidence in microbiome and bowel cancer. I hope my fellow science nerds enjoyed it. If that’s not you and you feel way in over your head, don’t stress! Over the next few weeks I will be sharing some more simple and practical tips, including how to take the above two methods on board. They will be actionable ways to help you eat your way to a healthier gut!
If you haven’t had enough of the science and still want to learn more, check out the further reading below!
腸道健康:人體消化道微生物(腸道細菌) 與腸癌
他們有甚麼關係和我們如何降低患上的風險?
正巧本月份是腸癌關注月,我將會寫我第一篇網誌關於腸道健康,特別有關於人體消化道微生物(腸道細菌) 。
你知不知道腸癌在澳大利亞是所有癌症種類內第二普遍?被診斷出患有腸癌的病例中,有30%的病人是因為家族遺傳。除了遺傳因素,最近有研究指出某些人體消化道微生物(包括口腔)亦會影響到我們患有腸癌的風險。
人體消化道微生物是一種細菌生存在消化管道內,從口腔到直腸。人類的腸道大約有一百萬億的微生物,幫助我們腸道維持一個良好的環境。不同類型和數量的微生物能夠導致不平衡的腸道環境,這不只影響消化功能,還有引起一些病徵,例如:便秘,腹瀉和腹脹。
人類的腸道大約有一百萬億的微生物,幫助我們腸道維持一個良好的環境。
儘管我們體內可能天生有著不同種類的微生物(基於不同基因和父母的生活模式),這些腸道細菌會定期改變。日常飲食便是一種重要因素能夠影響腸道內細菌的種類和數目。
舉一個例子,有研究者比較歐洲兒童和非洲兒童的飲食習慣,最主要的差異是歐洲兒童的腸道內有更多不同種類的細菌;非洲兒童則比較少。歐洲兒童有多種的腸道細菌一些能夠抗炎,一些能夠保護腸道,防止腸癌。
另外,Yang & Yu從許多以人類和動物的研究中收集了不同的結果,發現纖維,蛋白質和脂肪吸收是最主要影響腸道微生物的因素。重要理據包括:
- 當纖維在大腸內發酵會生產短鏈脂肪酸(SCFAs),特別是丁酸酯(丁酸鹽)。這行為會給予大腸內的細胞足夠的營養和促進抗炎的功能。
- 多吸收動物蛋白質不會改變微生物的多樣性,但會引致蛋白質發酵和膽汁酸早期解離,即是會增加大腸發炎的機會。
- 當習慣進食一些高脂肪的食物,特別是經過處理的肉和紅肉,會增加膽汁酸的釋放溶量,這會損害大腸內壁。
- 學術界在食用經過處理的肉和紅肉會否增加導致腸癌的風險存有分歧,然而,現時大多證據都偏向指出是會增加患癌風險
似乎微生物多樣性是對於幫助降低患上腸癌是非常重要,因為這能夠降低大腸發炎的可能性。我們可以做甚麼去增加腸道細菌的數量和種類從而降低發炎的機會?
跟據上述研究,有兩種關鍵方法:
-
增加進食纖維
-
減少進食經過處理的肉類和紅肉
References & Further reading
Bowel Cancer Australia. (2017). About Bowel Cancer. Retrieved from Bowel Cancer Australia: https://www.bowelcanceraustralia.org/what-is-bowel-cancer
Dahmus, J., Kotler, D., Kastenberg, D., & Kistler, C. (2018). The gut microbiome and colorectal cancer: a review of bacterial pathogenesis. Journal of Gastrointestinal Oncology. 9(4):769-777. Accessed from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6087872/
Filippo, C., Cavalieri, D., Di Paola, M., Ramazzotti, M., Poullet, J., Massart, S., Collini, S., Pieraccini, G., & Lionetti, P. (2010). Impact of diet in shaping gut microbiota revealed by a comparative study in children from Europe and rural Africa. Proceedings of the National Academy of Sciences of the United States of America.107(33):14691-14696. Accessed from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2930426/
Flemer, B., Warren, R., Barret, M., Cisek, K., Das, A., Jeffery, I., Hurley, E., O’Riordain, M., Shanahan, F., & O’Toole, P. (2018). The oral microbiota in colorectal cancer is distinctive and predictive. Gut.67(8). Accessed from https://gut.bmj.com/content/67/8/1454.info
Food and Mood Centre. (2016). Diet and the gut microbiota. Retrieved from https://foodandmoodcentre.com.au/diet-and-the-gut-microbiota/
Yang, J., & Yu, J. (2018). The association of diet, gut microbiota and colorectal cancer: what we eat may imply what we get. Protein & Cell.9(5): 474-487. Accessed from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5960467/